Managing a bifocal deformity with TSF◇
David Goodier, FRCS; Royal National Orthopaedic Hospital, UK
The views and opinions expressed in this section are those of the surgeon.

Introduction
Bifocal techniques involve two separate foci of treatment in the same limb segment such as multi-apical bony deformity correction, or correction of a bony deformity with adjacent joint contracture (typically an ankle equinus). In these cases two attached TSF constructs (“stacked frames”) can provide simultaneous correction.
Other indications include segmental transport where one focus involves closing a zone of bone loss, and the other focus is the lengthening site, as well as some cases of a tibial mid-shaft deformity with severe associated shortening, where there may be concern about gaining length at a diaphyseal osteotomy site. In this scenario one osteotomy can be used for the deformity, and a metaphyseal osteotomy used to regain length.
These latter cases can be managed with a hybrid construct using TSF at the docking site and classic IlizarovTM Threaded Rods proximally, or stacked frames can be used.
Deformity analysis
Multiapical deformities need careful systematic analysis to avoid the common pitfall of correcting an “obvious” mid-shaft deformity and leaving an overall malalignment. The method described in Paley’s “Principles of Deformity Correction”1 is used to identify the number of apices of deformity. Rotational abnormalities are difficult to assess radiologically, and almost impossible if associated with angular deformity due to change in the reference axis (“parallactic homologues”) so however accurate the planning, a residual correction is often necessary.
Case example
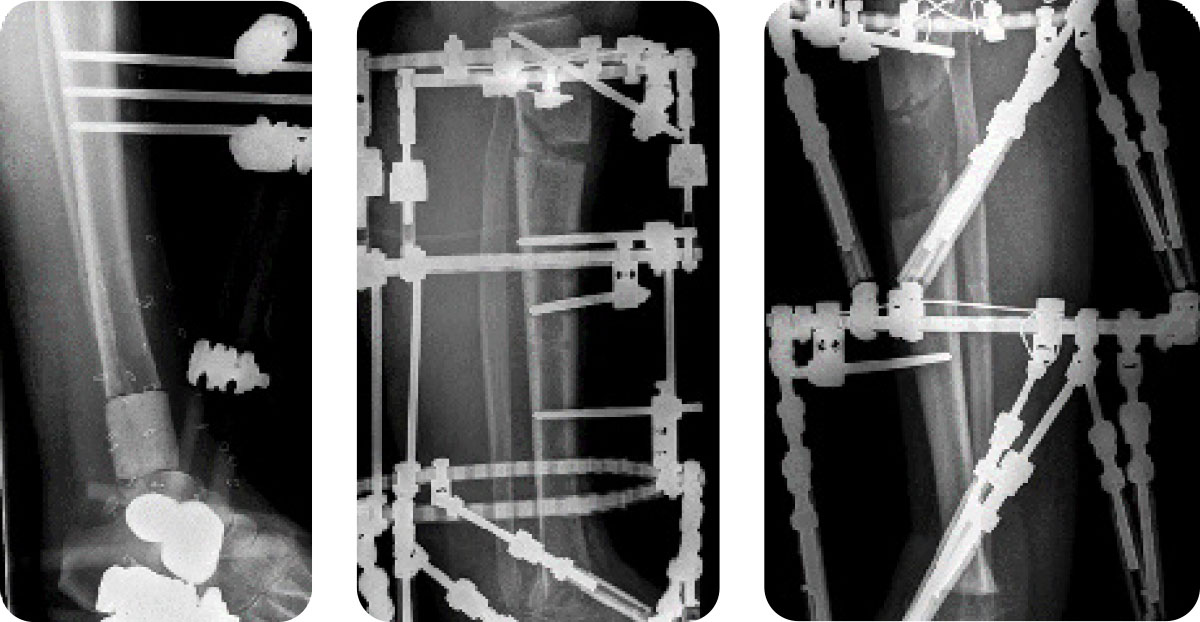
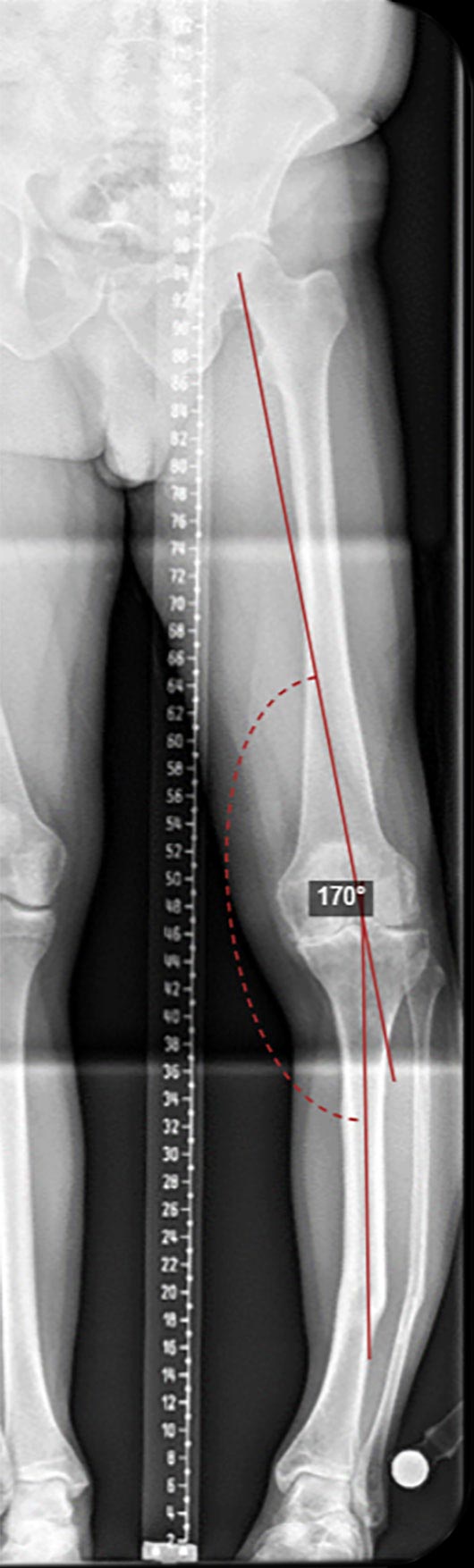
In this example the AP view shows there is overall varus and shortening, and a ‘“view” at the ankle with an AP knee confirming internal rotation. An extension of the proximal mechanical axis (blue line) and a reconstructed distal mechanical axis (red line) show a CORA outside the bone.
Resolving this with a best fit third line (magenta line) reveals a CORA at the diaphyseal “obvious” deformity and a hidden CORA at the joint level due to varus osteoarthritis. Correcting only at the obvious apex would leave significant residual overall varus. Sagittal planning shows translation, angulation and shortening at the diaphyseal obvious apex.
Two separate osteotomies, each corrected by a separate spatial frame, are necessary. The diaphyseal osteotomy will be through remodelled, cortical bone so regaining length would be best achieved at a proximal osteotomy.




Frame construction
There are two main choices when planning stacked frames; whether to use two completely separate frames and link them with hexagonal sockets or threaded rods, or to create a three-ring construct where the middle Ring is common, and hence the distal Ring of the proximal frame, and the proximal Ring of the distal frame.
The use of a common Ring reduces the number of holes available for fixation elements; this is particularly problematic if wires are used where all six tabs are occupied by Struts. SMART TSF◇ Rings and Custom Strut Mounting possibilities, however, significantly reduce this problem by the ability to move the Strut positions to adjacent unoccupied holes.
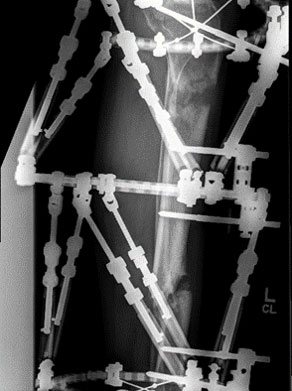
The example shown may be considered for management of a proximal and distal deformity.
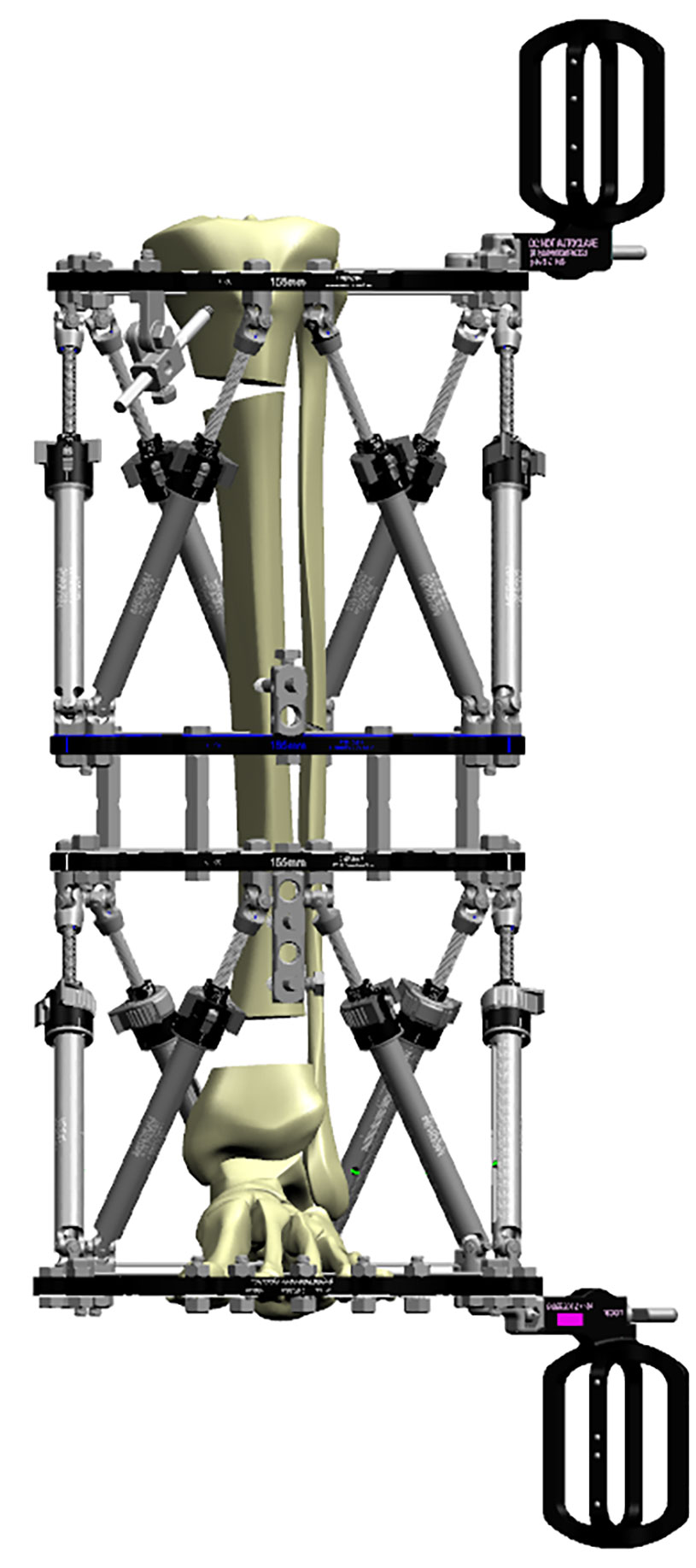
This construct shows a proximal frame with ILIZAROV Graduated Telescopic Rods driving axial translation only. Excision of a defect and acute shortening are performed distally. The TSF is used to achieve accurate reduction at the docking site, while the proximal corticotomy is used to restore length.
When planning a frame for segmental transport, there are issues with “working length,” i.e., the mechanical concept of unsupported distance between fixation elements and the bone ends. The excised bone gap starts wide, but the Ring position must allow for docking of the bone ends. With classic TSF the minimum distance must be taken into consideration when planning; with SMART TSF and the use of 30mm Step-Off Plates there is no minimum distance between Rings. Similarly, if there is to be a long regenerate segment at the proximal end of a transport construct, the initial setup can use Step-Off Plates to allow a very short working length at the corticotomy site, then changed out to default Strut positions as the gap widens.
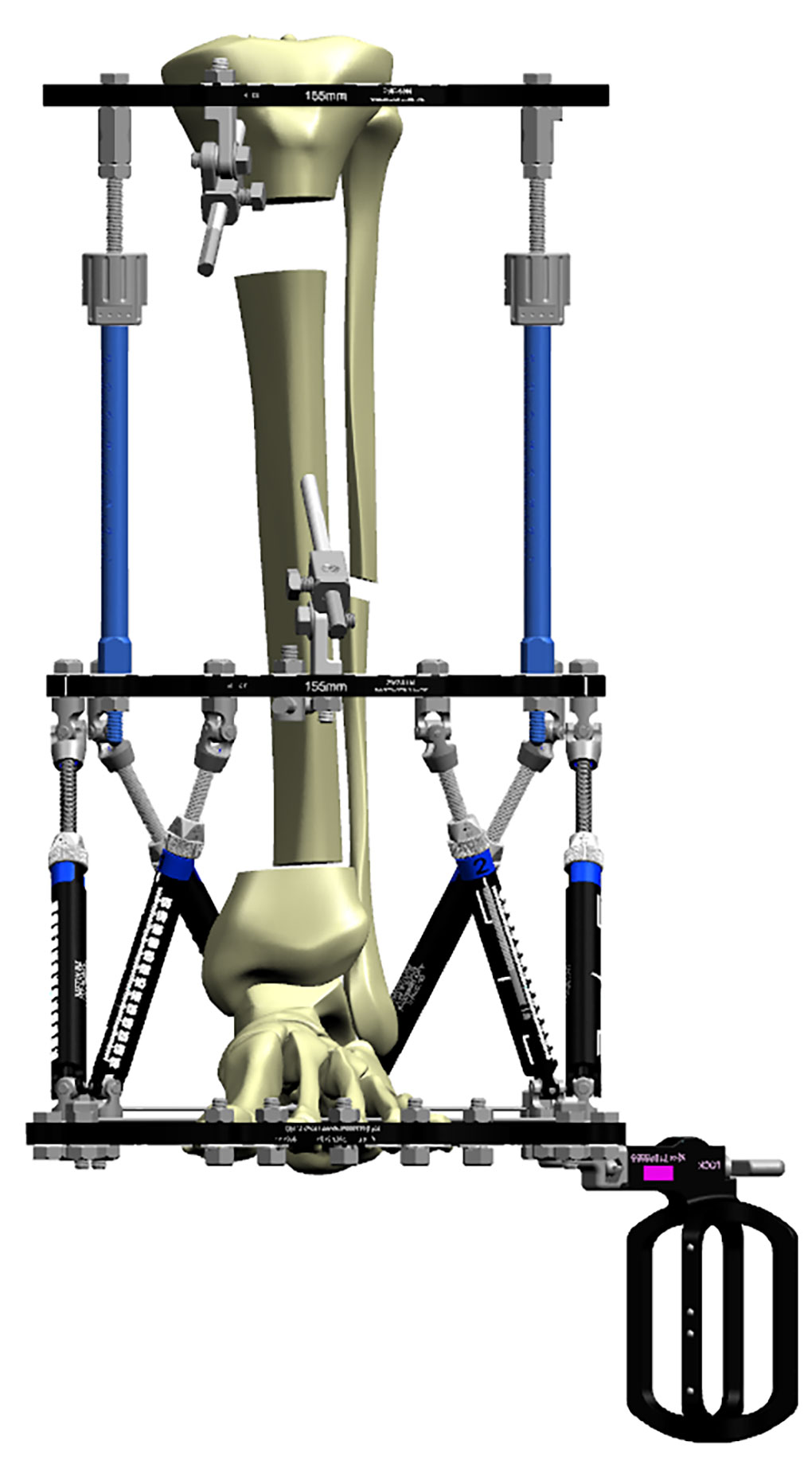
The most proximal Ring should be a 2/3 Ring to allow for knee flexion. In classical Ilizarov fixation “near and far” fixation in a segment can be accomplished using a two-ring block. The stronger TSF◇ rings allow the use of a single Ring, but a greater working length can be achieved by elements mounted off the Ring.
Classically a reference wire parallel with the articular surface above the Ring and below the reflection of the capsule of the knee joint is inserted first, followed by an oblique wire through the fibular head to prevent distal subluxation during lengthening.
An AP half pin can be inserted at the lower end of the tibial tubercle; if this is fixed off a Rancho Cube, then the penetration of the posterior cortex can be close to the corticotomy site and crack into it. For this reason, an oblique half pin is preferred, particularly as it can give a long length of bony fixation. The Angled Pin Connectors will fit between Struts 1 and 2 if the struts are outer mounted and the clamp mounted though the inner central hole. If the fixation hardware impinges against the Strut base, a custom strut mount can be employed.
Diaphyseal fixation is achieved mainly by half pins, again with a good spread of fixation by mounting proximal and distal to the Ring. A distal Ring is fixed by a wire to secure the distal tibio-fibular joint and other wires/half pins as indicated.
Osteotomies
When planning an osteotomy, bony remodelling should be considered, and the likely quality of regenerate. In the case above, a transverse osteotomy above, below or at the level of deformity will leave a large spur of bone that may cause soft tissue impingement, so an oblique osteotomy can be performed. The fibula must also be divided.

An osteotomy above the deformity causes a posterior bony lump, and likewise below causes an anterior spur. An oblique sliding osteotomy can allow correction of angulation but will prevent rotation at this level.
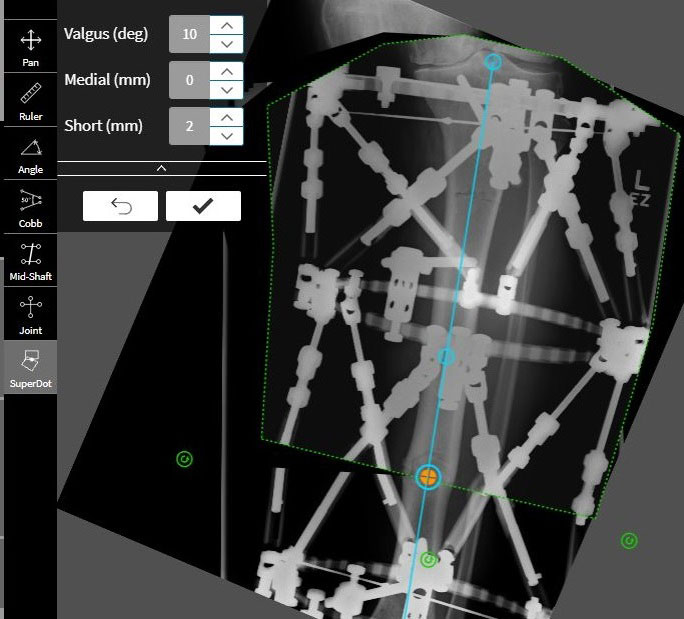
If the CORA is above the possible osteotomy level (as in the proximal tibia in this example) then Paley Osteotomy Rule 2 applies, i.e., the angulation can be corrected with translation. In this case there will be lateral translation to correct the joint line varus, as well as correction of rotation. Since this osteotomy is through metaphyseal bone, it is better to regain the majority of length here.
Software
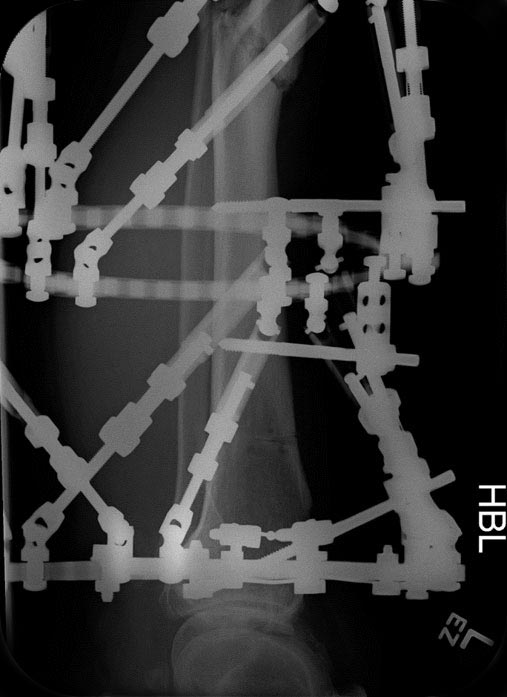
For a stacked construct, two separate programs are necessary. A Beacon Mount is attached to the most proximal and most distal Rings. Post-op X-ray images are taken with respect to each segment. SMART TSF◇ software does not require an orthogonal view of the Ring.
When planning for a translation at the osteotomy site, the planning can actually use the true CORA at the knee level, i.e., the origin and corresponding point can be placed proximal to the ring and without translation. If however there is shortening, then the true origin is virtual and lies along a line projected from the distal axis. This concept of an Extrinsic Origin is handled in SMART TSF by selecting Apex = Corresponding Point.
The parameters are entered into the software program, and a structure at risk identified (usually the fastest moving point on the regenerate) and a prescription generated. The patient is provided with two separate adjustment schedules, and monitored with appropriate radiographs as indicated until correction is complete.
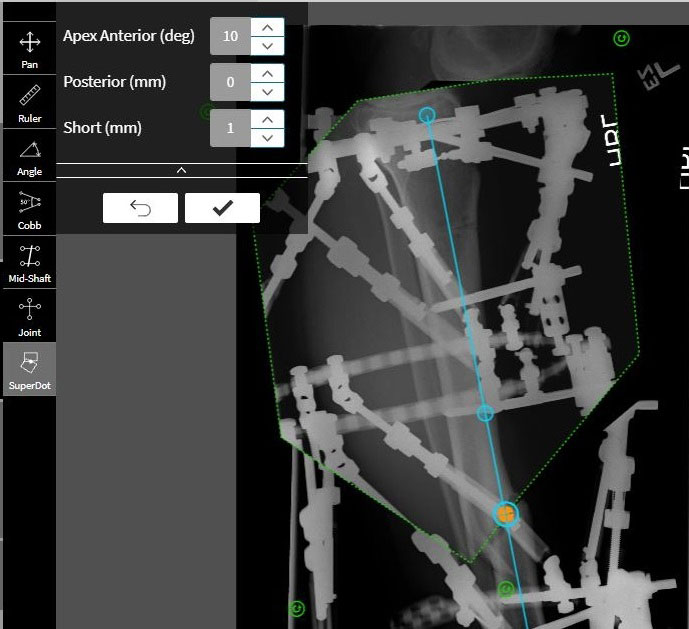
Using Osteotomy Sandbox for pre-operative planning
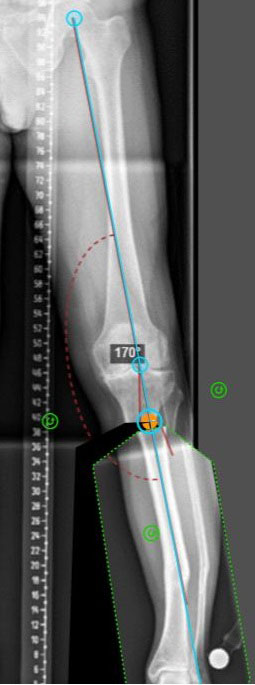
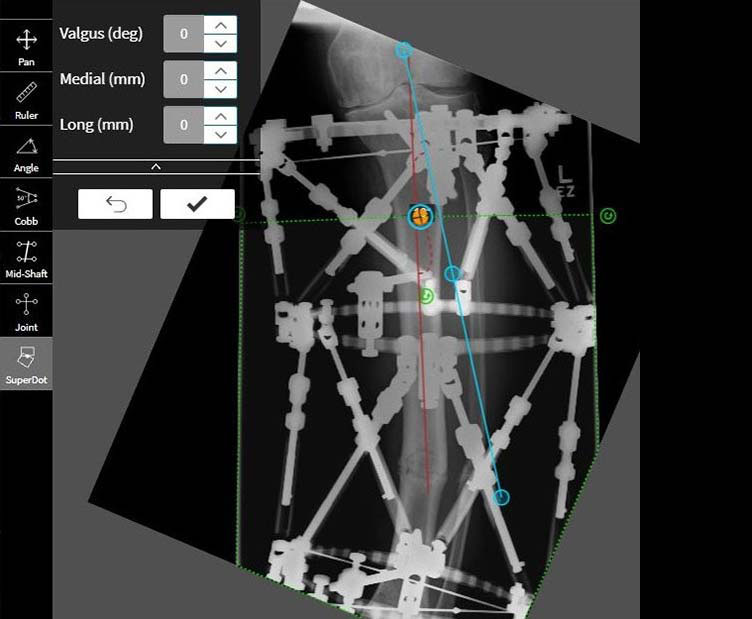
The Osteotomy Sandbox can be used to plan or play with the Osteotomy location before frame application.
- Bring in a full leg X-ray to the Osteotomy Sandbox
- Use Line tools and Angle Tools to draw the axes
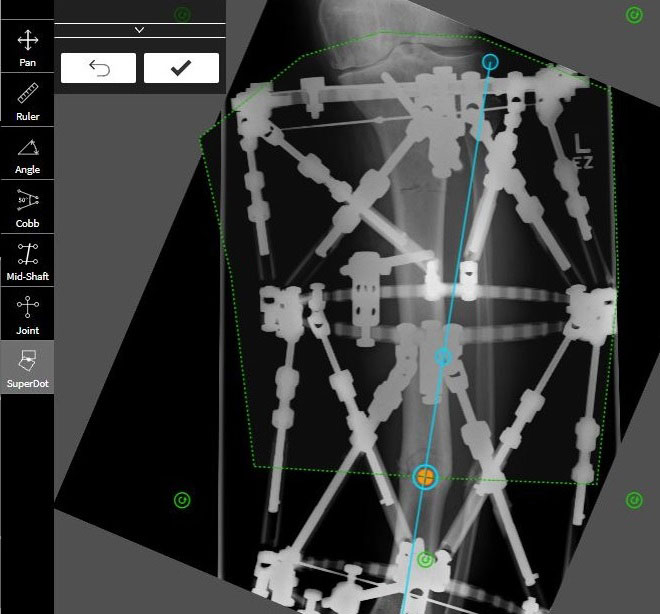
- Use SuperDot tool to trace out the moving fragment and cut the bone
- Place the SuperDot on the cut
- Use the handle to move the bone back onto the axis
- Download and save this image to an external folder
- Upload this image back to the Osteotomy Sandbox
- Repeat the anlaysis for the second deformity



Post-operative software analysis
Proximal deformity
The moving fragment is traced out and the SuperDot placed on the osteotomy. The bone is restored to the mechanical axis.
Analysis is performed on the Lateral, regardless of whether any sagittal plane deformity exists.
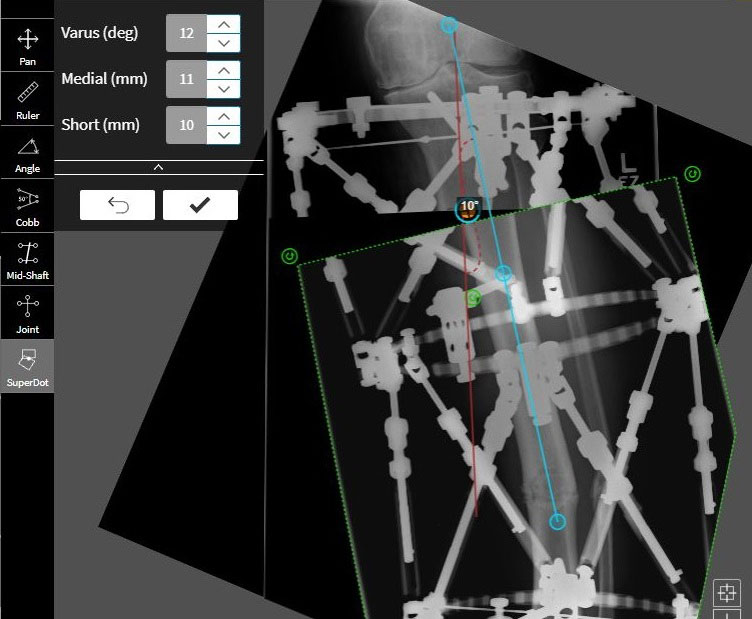
Distal deformity
The moving fragment is traced out and the SuperDot placed on the osteotomy. The bone is restored to the mechanical axis. Analysis also performed on the Lateral.
The patient will have two Prescriptions, one for each TSF.◇
Post correction
There is apparent residual shortening, but the femoral length confirms this is artefactual foreshortening due to knee flexion. The hip/knee/ankle alignment axis has been slightly over-corrected to offload the medial compartment.
Consolidation is monitored by serial radiographs, and usually occurs at one site before the other allowing partial dismantling of the frame prior to complete union. With modern pin-site care, infection is rare and is usually controllable with a short course of oral antibiotics.
Physiotherapy should ideally start preoperatively to work on muscle length and joint range of movement, and continue throughout and after treatment. Most frame constructs allow weight bearing as tolerated except in the most obese patients.
Night splintage to prevent ankle contractures is usually sufficient, but if an ankle deformity is being corrected distally, it may be necessary to pass K-wires through the toes to prevent contracture.
Frame removal can be either under anaesthesia, sedation, or with gas analgesia in an outpatient setting. It is rare for regenerate to fracture suddenly but it may plastically deform if frame removal is too early. For this reason it is possible to remove or unlock Struts and allow mobilisation for a week or two; if deformity occurs, it is easy to replace the struts and correct the deformity; if not, the frame can be removed with confidence without the need for additional splintage.

References
- Paley, Dror. Principles of deformity correction. Springer Science & Business Media, 2002.